With years of experience under its belt, MIT Medical works with the campus community to limit the spread of Covid-19.
Contact tracing is an essential tool for fighting the Covid-19 pandemic: If someone tests positive for the virus, health care workers move quickly to determine who else the infected individual had close contact with, and to set up measures to keep the virus from potentially spreading further. Yet while contact tracing has been a much-repeated phrase during the pandemic, people in the MIT community and beyond may wonder: How does the system actually work on the Institute’s campus?
As it happens, MIT runs its own swift-moving contact tracing program through MIT Medical, the campus’ health center — which delivers test results and exposure information to individuals affected by positive cases, and helps them chart their next steps as they quarantine.
“It allows for us to help the community very quickly, get notifications out, and give support to individuals,” says Shawn Ferullo, associate medical director and chief of student health at MIT Medical. Ferullo, Nurse Practitioner Jacqueline Sherry, and Nurse Practice Manager Maura Rowley have been leading MIT’s contact tracing program.
In handling this process during the Covid-19 pandemic, MIT Medical’s team members are drawing on years of contact tracing experience, applied to limit the spread of chicken pox, measles, mumps, tuberculosis, and other infectious diseases. Sherry, who specializes in occupational medicine and infectious diseases, has also developed a long-running relationship with the Cambridge, Massachusetts Department of Public Health, which ultimately oversees regulations and procedures for the city.
That know-how has helped MIT Medical set up a contact tracing program for Covid-19 with high priority on immediate action.
“Contact tracing work is today’s work today,” Ferullo notes. “This isn’t, ‘Oh, it’s 5:00 p.m., we’ll get to it tomorrow.’ The work day doesn’t end until the work is completed.”
Action after positive tests
So far 39 members of the MIT community have tested positive for Covid-19, based on the tests administered by MIT since August. The Institute tests MIT students, faculty, and staff at regular intervals on campus. Community members can also get tested if they are experiencing Covid-like symptoms.
The MIT tests are collected at one of MIT Medical’s testing sites and are processed at the Broad Institute. Depending on the reason for the test, community members receive test results via either the Covid Pass app (where they also enter their daily health attestations and get reminders for routine campus testing); or MIT Medical’s electronic medical record patient portal, if the test was performed as part of a clinical care visit.
When a positive result occurs, a small number of MIT Medical personnel are notified, and one of them quickly contacts the individual in question by phone. If the patient does not pick up, a non-specific message is left via voicemail — and, in some cases, email — urging them to contact MIT Medical right away.
“Step number one is always notifying the person who has the result, so they’re aware right away and know they should isolate,” Ferullo says. “We [want to] catch them before they go in to work, or before they go to class. Some of that call is support for that individual too.” When people test positive, he adds, they usually ask: “‘What does this mean? How did I get this?’ There’s a little bit of helping them digest the result, [asking if they] live with family members, and how can we help them. That call happens right away.”
People testing positive must then enter into a period of isolation for a minimum of 10 days, rigorously limiting contact with other people.
At the same time, MIT Medical’s contact tracing team also works with the individual who has tested positive, to trace their recent activities and identify any close contact with other community members. That information sparks a second round of phone calls: The MIT Medical team then talks to the people (if there are any) who may have been exposed to the virus by the Covid-positive individual.
If that level of contact was significant enough, the exposed individuals also have to enter into a 14-day quarantine. For these people — who do not know if they have contracted the virus — MIT Medical recommends that they have a Covid-19 test approximately five to seven days from the time of contact, when about 99 percent of people carrying the virus will test positive. Even if that day 7 test is negative, though, people still must observe quarantine for 14 days, by state regulations.
When people must quarantine due to exposure to a positive-testing individual, MIT Medical staff will give them direction to help figure out the logistics, just as the staff will work with people who have tested positive.
“We talk them through what it means for them, and offer them that same support, all the appropriate guidance,” Ferullo says.
MIT Medical strictly follows all privacy regulations: When communicating with people who may have been exposed, they do not disclose the name of the individual who tested positive. Through all of this, speed is essential.
“We had someone who tested at 10:30 in the morning, we got their positive result from Broad at 5:30 in the evening, and by 6:30 all the contacts were done and all the notifications of other individuals were done,” Ferullo says. The faster people can begin quarantining, the lower the transmission rate in the community, in all likelihood.
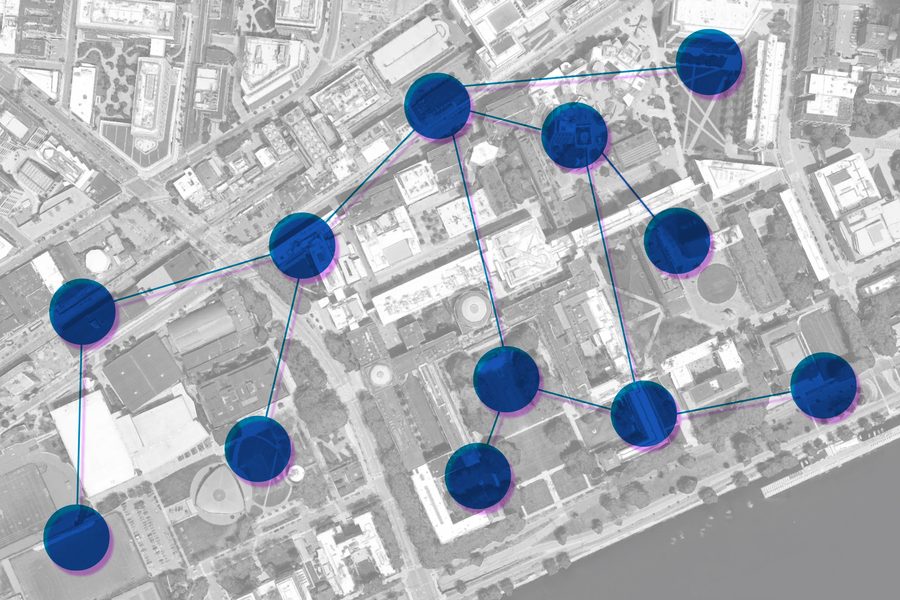
Additionally, once the positive individual has been notified and their contacts have been established, the contact tracing team reviews the spaces on campus that had been used by the positive individual in the previous 48 hours.
“We recognize that contact tracing is first and foremost about the notification of the individual, identifying any people with whom they have had close contact, and then considering the space that had been used,” Ferullo says.
Through close partnership with campus partners in MIT Emergency Management; the Environment, Health, and Safety Office; Custodial Services; and MIT Facilities, the contact tracing team establishes details about spaces that require a rapid, efficient cleaning, as per the Institute’s Covid protocols. The identity of the positive individual is again kept private during this process, while the needs assessment is shared and the cleaning is done.
Continued support
MIT Medical has built layers into their contact tracing team, and has trained more staff to be activated to help to handle contact tracing, should the MIT case load increase. So far, only the core team has been called into action. But all of them are ready if needed.
Contact tracing can be labor-intensive: When people test positive, the contact tracing team will follow up with those individuals the next day by phone, and do the same for people who have had close contact with them.
“We do that so we can continue to offer them support, recognizing that oftentimes people will hang up and then think of questions they couldn’t think of in the moment,” Ferullo says. “I feel we can do it in a way that we can really support our community members. You don’t want people to hang up that phone and then think, ‘Now what?’”
So far, Ferullo notes, “The biggest challenge sometimes is reaching individuals, if they don’t answer their phone or have voicemail set up.” In those cases, staff will send emails to community members, asking them to answer their phones if MIT Medical calls. Due to privacy regulations, MIT Medical does not disclose substantive information in emails.
At the same time, Ferullo praises the attitude the MIT community has taken during the pandemic, noting how much efforts to contain the virus are helped by strict adherence to safety protocols.
“I will say, when you’re doing contact tracing, you realize the power of physical distancing and mask policies,” Ferullo says. “The best [cases] are when people have zero close contact, because they did all the right things. … I think what we see is how those policies quickly feed into controlling spread of the virus.”
Ultimately, he notes, MIT Medical’s goal is to serve people, and their complex needs, at a time when the Covid-19 pandemic has already complicated daily life.
“Every case is different,” Ferullo says. “Because every person is different, every life is different. Who has young kids at home? Who cares for their elderly parents who live with them? Who needs to be in a lab? Who lives in a dorm room by themselves? So each case has a flavor of the same, but they’re all very different. We see our role as not just notifying and manging, but supporting and helping navigate, too. I think we’re trying to do all those things at the same time for the community.”